Measurement-based care impact study reveals a clinical impact on adverse events—resulting in a 28% reduction in total cost of care for Colorado health plan


INTRODUCTION
Aurora Mental Health & Recovery (AMHR) is a certified community behavioral health clinic committed to using measurement-based care (MBC) to get their clients better, faster. Their payor, Colorado Access, was interested in their positive outcomes. With Owl, they embarked on an innovative collaboration to analyze client spend, utilization, and outcomes across patient cohorts and timelines over two years. The results demonstrated that measurement-based care with Owl has a clinical impact on adverse
events while reducing cost.
Measurement-based care impact study key results
Aurora Mental Health & Recovery and measurement-based care
“Ultimately, we chose Owl as our partner. From high rates of patient and clinician engagement to completely automating measurement-based care to the data insights that help us improve care, Owl offers everything our organization needs.”
About Aurora Mental Health & Recovery
About Colorado Access
About Owl
Measurement-based care impact at Aurora Mental Health & Recovery
Clients are highly engaged
AMHR achieves an 87% patient engagement rate.
Clients get better, faster
Clients at AMHR achieve a 56% faster time to remission compared to clients not engaged in measurement-based care.
Opportunities to expand access with existing resources
Not only is AMHR getting patients better faster, but they also have data insights to help understand which patients have reached remission and recovery—revealing 30% of patients may be ready for stepped-down care or discharge.
Quick responsiveness to suicidal ideation and self-harm alerts
Owl alerts the AMHR team of patients with suicidal ideation or those at risk for self-harm. Over 90% of these alerts result in a new or modified schedule change within a week of the alert, indicating that AMHR staff immediately responded to maintain the safety and well-being of their clients.
To learn more, read the entire Aurora Mental Health & Recovery case study
Results caught the attention of Colorado Access
The published results of AMHR’s MBC implementation with Owl caught the attention of Colorado Access, the largest public sector health plan in the state. While Colorado Access utilizes a several different value-based models in their provider network, implementing value-based reimbursement models in behavioral health has been challenging. Using claims data doesn’t provide the quality of care or the outcomes of services delivered by their network providers.
Senior Director of Behavioral Health Network Performance, Colorado Access
Measurement-based care data impact study
The Results
Reduced IP admits
Consistent Owl users show a 75% reduction in psychiatric IP admits. The control group displays no significant change.
Reduced ER visits
Consistent Owl users show a 63% reduction in psychiatric ER visits. Control group displays no significant change.
Per member per month savings
Consistent Owl users display a 28% PMPM decrease versus the control group.
Measurement-based care impacts total cost of care
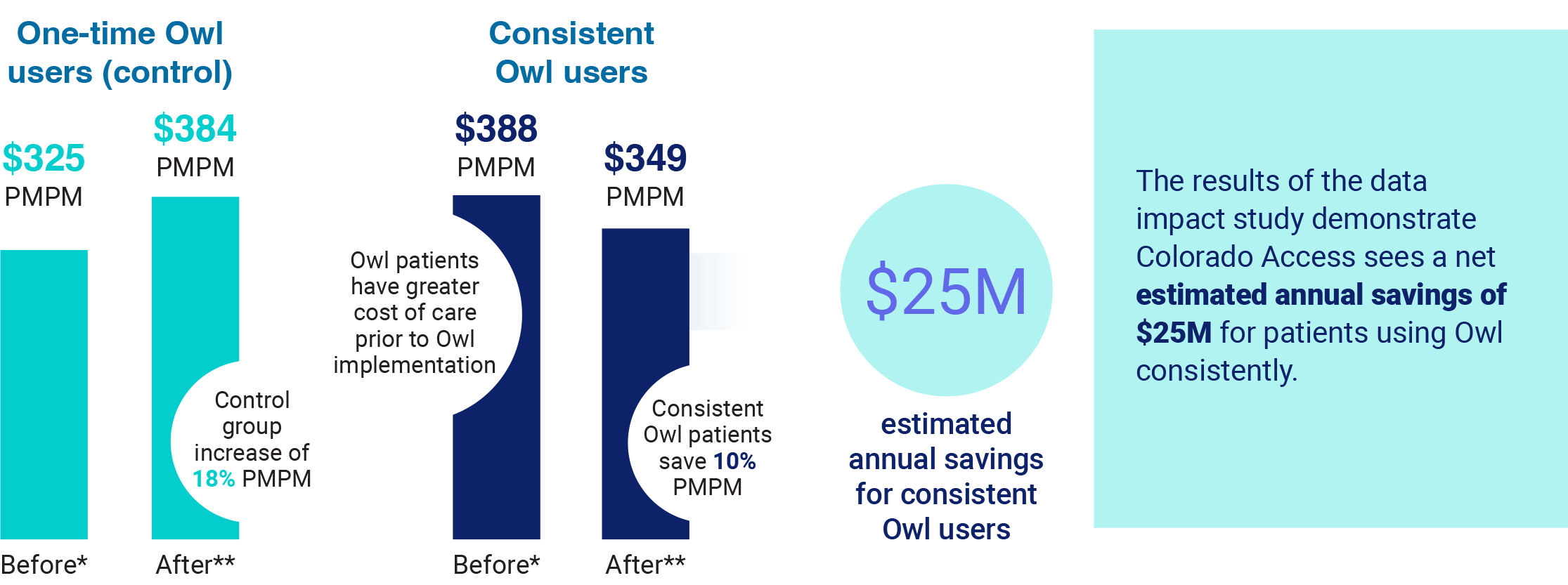
The data overwhelmingly supports what research has shown for decades—measurement-based care improves patient care and clinical outcome while significantly reducing the cost of care.
Research has consistently shown that the practice of measurement-based care (MBC) improves patient outcomes among various treatments, populations, and settings. It also shows MBC enhances clinical decision-making and quality of care, enriches communications between patient and provider, and can demonstrate the value of treatment.
The collaborative efforts between AMHR, Colorado Access, and Owl validate the significant impact of MBC on both patient outcomes and cost savings. By integrating MBC into their care delivery model, AMHR has not only improved treatment effectiveness but also positioned themselves favorably for value-based reimbursement discussions with payors like Colorado Access.
For the first time ever, Colorado Access has real-world data on treatment outcomes and associated costs to build value-based and alternative payment models that incentivize and attract providers to deliver high-quality, cost-effective care to their members.

Better engagement in behavioral health care leads to total cost of care savings across the healthcare spectrum
To learn more about the measurement-based care impact study or how Owl can help your payor or provider organization get the outcomes data you need to improve outcomes and significantly reduce costs, contact us.
